Each year, the flu sickens millions of people worldwide, and it can become far more dangerous when certain bacteria in the lungs join the infection. These co-infections can lead to pneumonia and other serious complications, but scientists still don’t fully understand why some combinations of germs make the illness worse.
To study the problem, a team co-led by Julia Oh, PhD, a microbiologist and professor of integrative immunobiology at Duke School of Medicine, and Ibrahim Ozbolat, PhD, of Penn State, has received a four-year, $3.2 million grant from the National Institutes of Health.
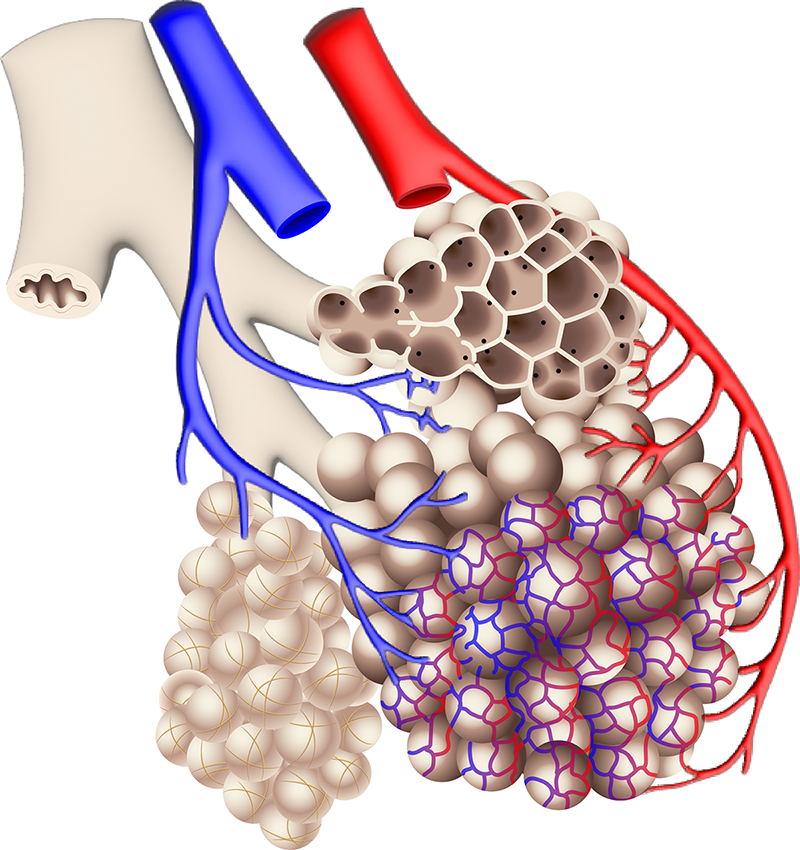
Scientists will study how different bacteria interact with the flu virus in human lung tissue, using a 3D-printed lung model that closely mimics how real lungs function.
“Researchers have long studied the flu virus’s effects on the lungs, but we don’t know how adding diverse bacterial strains changes the outcome,” said Oh, the project leader. “The respiratory microbiome varies widely between people, and we’ve lacked models that reflect that complexity.”
The team will use a 3D-bioprinted lung model developed in Ozbolat’s lab. Made from stem cell–derived lung cells, the tiny tissues can be ventilated like real lungs, letting scientists add viruses and microbes and watch infections unfold in real time.
“The precision of bioprinting lets us recreate miniature, breathing lung sacs that behave like native tissue,” Ozbolat said. “This is the first time a dynamic 3D lung model will be used to study virus–bacteria interactions.”
Ozbolat’s team will create the tissues at Penn State, while Oh’s Duke group will introduce influenza and select microbes. Using multiomics and advanced imaging, they aim to uncover why some co-infections intensify illness and why others may help prime immune defenses.
Because influenza is so widespread, the researchers say the findings could inform future vaccines and treatments — and the platform could transform how respiratory diseases are studied without relying on animal models or human infections.
The team includes collaborators from the Jackson Laboratory and Nationwide Children’s Hospital.