Researchers in Maria Ciofani's lab, studying multiple sclerosis in mice, have identified a protein that could reshape the understanding of MS treatments.
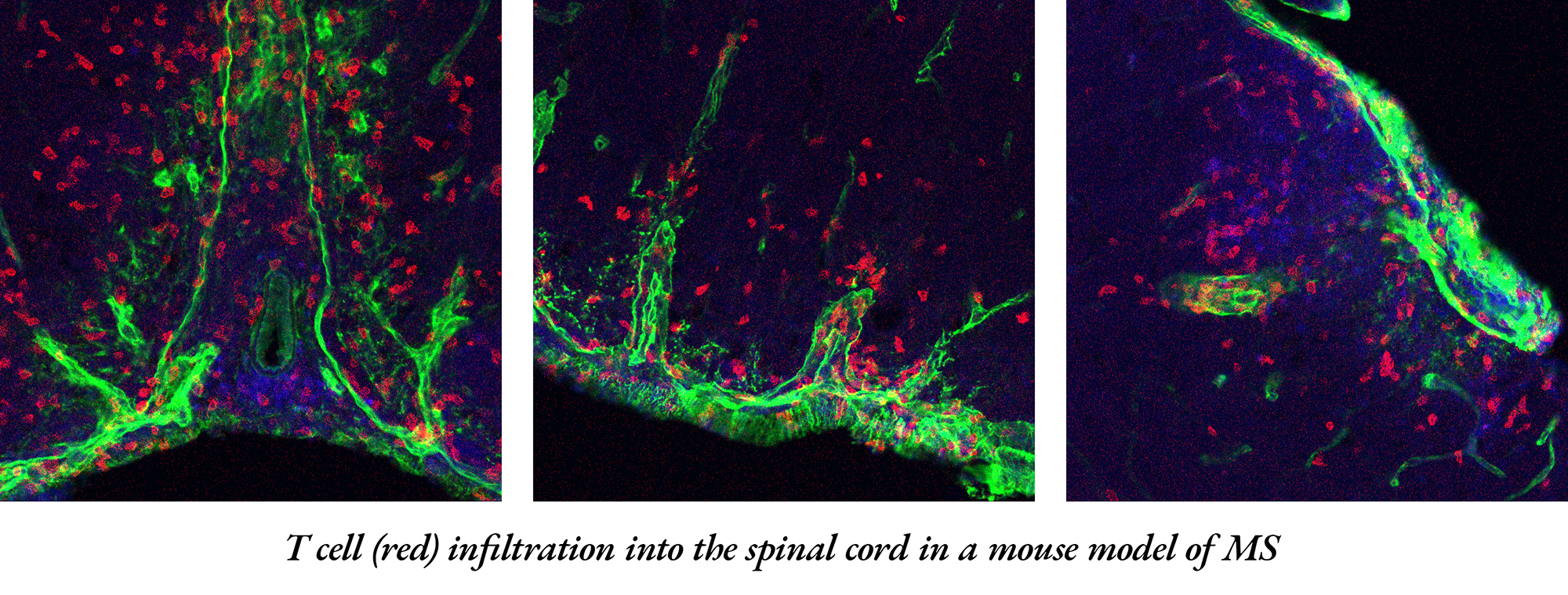
The protein boosts the aggressive migration of immune cells into the central nervous system, leading to MS, an autoimmune disease affecting about 1 million adults in the United States. The intrusion of a specific type of immune cell called Th17 is particularly harmful to the brain and spinal cord.
But when Duke scientists blocked the protein -- integrin α3 – it slowed immune cells from reaching and damaging the central nervous system and improved symptoms in mice, according to a study appearing online Oct. 13 in Science Immunology.
“We were studying the role of another gene when we stumbled upon integrin α3,” said co-lead author Maria Ciofani, Ph.D., associate professor in Duke’s Department of Integrative Immunobiology. “We found that when it’s missing, the Th17 cells don’t develop as effectively, and more importantly, they face difficulties entering the central nervous system. This means less damage.”
The Th17 cells, which are vital for the body to fight fungal and bacterial infections, don’t usually cause diseases. But for people with MS, these cells are mistakenly activated and end up attacking the central nervous system.
The Duke team is the first to reveal the abundance of integrin α3 on Th17 cells. The protein helps Th17 cells to form connections with other cells, which in turn helps the cells grow and become more aggressive.
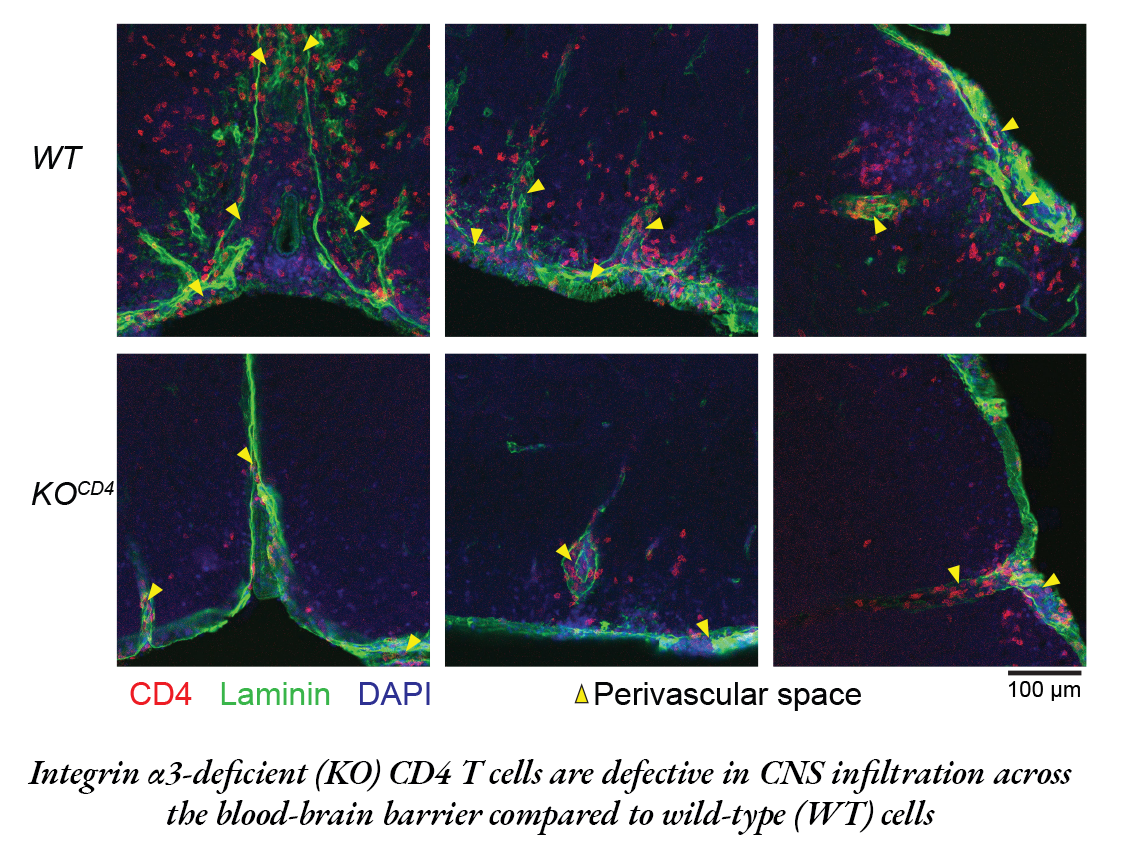
But in the absence of the protein, Th17 cells get trapped outside the blood-brain barrier, the brain’s protective shield.
While probing inflammatory T cells and disabling a particular gene -- a routine practice to grasp its function -- researchers stumbled upon a surprise. The altered mice were fully shielded from the MS-like symptoms typically seen in such models.
“They were walking around like nothing happened,” Ciofani said. “When we looked carefully, we found that none of the Th17 cells were entering the central nervous system. It was an opportunity to look at the machinery that controls these cells.”
With the help of computational approaches, Ciofani's team -- including co-lead study author Eunchong Park, Ph.D., -- identified integrin α3. Park, a scientist at AstraZeneca, is a former graduate student in the Department of Integrative Immunology and a member of the Center for Advanced Genomic Technologies.
There’s currently no drug that targets integrin on Th17 cells, but the drug natalizumab does target another kind of T-cell, Th1, that can also cause MS. But natalizumab has its side effects, emphasizing the need for alternative treatments.
“One concern about targeting integrin α3 is that these Th17 cells are vital for our body’s defense against infections,” Ciofani said. “We’ve done preliminary tests to see if inhibiting integrin α3 stops Th17 cells from doing their protective roles, and so far, it seems they can still do their jobs.”
Since integrin α3 is so essential for the harmful actions of Th17 cells, it could be a potential target for new MS treatments.
Additional Duke authors include William E. Barclay; Alejandro Barrera; Tzu-Chieh Liao, Harmony R. Salzler; Timothy E. Reddy; and Mari L. Shinohara.
The study received funding support from the National Institute of Health (R01-GM115474, R01-AI156186, R01-NS120417, RG-4536B2/1, UM1-HG009428) and a Kwanjeong Educational Foundation Scholarship.
Written by Shantell M. Kirkendoll, this article originally appeared on the Duke School of Medicine website.